Common virus may be celiac disease culprit
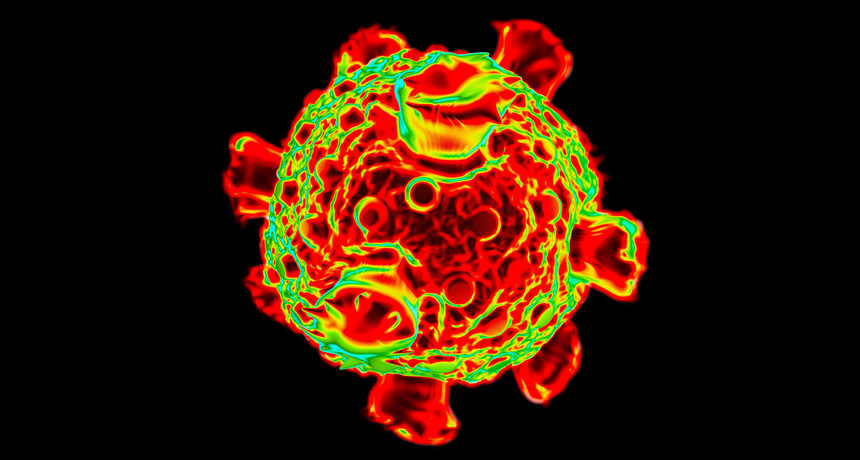
A common and usually harmless virus may trigger celiac disease. Infection with the suspected culprit, a reovirus, could cause the immune system to react to gluten as if it was a dangerous pathogen instead of a harmless food protein, an international team of researchers reports April 7 in Science.
In a study in mice, the researchers found that the reovirus, T1L, tricks the immune system into mounting an attack against innocent food molecules. The virus first blocks the immune system’s regulatory response that usually gives non-native substances, like food proteins, the OK, Terence Dermody, a virologist at the University of Pittsburgh, and colleagues found. Then the virus prompts a harmful inflammatory response.
“Viruses have been suspected as potential triggers of autoimmune or food allergy–related diseases for decades,” says Herbert Virgin, a viral immunologist at Washington University School of Medicine in St. Louis. This study provides new data on how a viral infection can change the immune system’s response to food, says Virgin, who wasn’t involved in the study.
Reoviruses aren’t deadly. Almost everyone has been infected with a reovirus, and almost no one gets sick, Dermody says. But if the first exposure to a food with gluten occurs during infection, the virus may turn the immune system against the food protein, the researchers found.
The immune system can either allow foreign substances, such as food proteins, to pass through the body peacefully, or it can go on the attack. In people with celiac disease, gluten is treated like a harmful pathogen; the immune system response damages the lining of the small intestine, causing symptoms like bloody diarrhea.
Celiac disease has been associated with two genetic features. Though 30 to 40 percent of people in the United States have one or both of these features, only 1 percent of the population has been diagnosed with the disease. This disparity suggests that some environmental factor triggers it.
Dermody and colleagues found that the T1L reovirus may be a trigger. In mice engineered to have one of those genetic features, the virus appeared to trick the immune system into seeing gluten as an enemy.
The key interaction occurs in the mesenteric lymph nodes, where gluten meets up with dendritic cells, which are like the “orchestra conductors” of the immune system, Dermody says. These cells dictate whether the immune system ignores a substance or mounts a defense against it.
But the virus engages with the dendritic cells as well, fooling the cells into thinking that gluten, like the virus, is in some way dangerous. And then the immune system attacks the gluten.
Dermody and colleagues also found that the reovirus stimulated activity of an enzyme called tissue transglutaminase. In people with celiac disease, the enzyme makes gluten more able to trigger a harmful immune system response.
Celiac patients also had higher levels of reovirus antibodies than those found in people without the disease.
Dermody doesn’t think that the T1L reovirus is the only virus that can stimulate celiac disease. Future research will analyze the potential of other viruses and also determine whether T1L is a true trigger of the disease in humans. If it is, then a reovirus vaccine could be developed for at-risk children, which could potentially block the development of celiac disease, “and that would be pretty amazing,” Dermody says.