A universal flu shot may be nearing reality

One of the planet’s deadliest viruses makes an annual pass through the United States with little fanfare. It rarely generates flashy headlines or news footage of health workers in hazmat suits. There’s no sudden panic when a sick person shows up coughing and feverish in an emergency room. Yet before next spring, this season’s lethal germ will probably have infected millions of Americans, killing tens of thousands. Still, it’s often referred to as just the flu.
The influenza virus seems so normal to most Americans that only about half of us will heed those “time for your flu shot” banners that pop up at pharmacies and worksites every autumn. Those annual shots remain the best means of protection, but they must be manufactured months before flu season starts, based on a best educated guess of what strains of the virus will be circulating. That means even in a successful year, vaccine performance may not be impressive. During the 2015–2016 season, only about half of those immunized were protected, according to a study in the Aug. 10 New England Journal of Medicine. Some years’ vaccines are duds: For the 2014–2015 season, the vaccine protected only 19 percent of people who received it, based on U.S. Centers for Disease Control and Prevention data.
Scientists have long worked to develop a flu shot that works better and lasts longer. But, unlike the very stable measles virus, influenza is a moving target. While only a few strains of flu virus circulate worldwide in a typical year, dozens more may exist. Each one is highly likely to mutate from year to year, with just enough shape-shifting to be unrecognizable to the body’s defenses.
Now, after years of searching, scientists believe they have better strategies to attack the parts of the virus that stay the same from year to year, offering the hope of protection across multiple seasons. The vaccines being developed in laboratories around the world “offer more promise than we’ve ever had,” says Walter Orenstein, associate director of the Emory Vaccine Center in Atlanta. And there are new creative approaches: One research group is trying to make a kind of super shot by anticipating every possible mutation a circulating virus might undergo.
“I’m optimistic we are going to get to a vaccine,” says Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, or NIAID, in Bethesda, Md. Then, you may need to heed those “time for your flu shot” messages only once.
Researchers often describe the flu virus as looking like a ball with lollipops sticking out. Tucked inside the ball is RNA, which the virus needs to make copies of itself. The lollipops on the outside are proteins: hemagglutinin and neuraminidase. There are 18 different kinds of hemagglutinin and 11 kinds of neuraminidase. Each kind of flu virus is named for its particular combination of these proteins; the current forms circulating around the world are H1N1 and H3N2. Hemagglutinin attaches to human cells to launch an infection; neuraminidase is more important for spreading the virus once infection has occurred.
Flu viruses involved in human epidemics are divided into types A and B, and A viruses are sliced even further into group 1 and group 2. Influenza A, the most troublesome for vaccine scientists, travels the world among birds, pigs and humans. The bird and pig versions don’t easily infect people, but the virus is constantly mutating and even swapping genes with other influenza viruses it meets along the way. Sometimes these genetic changes create a version that allows a bird or pig flu to move directly into humans. In 2013, one called H7N9 moved into people in China (SN Online: 3/11/15). The virus has since infected more than 1,500 people. Mostly, though, the genetic changes are more subtle, with just enough alterations to evade the human immune system.
Like kids with a sweet tooth, the immune system gets most excited about the top part of the hemagglutinin lollipop, and makes antibodies against it. The top is, after all, the first thing the immune system notices once the virus slips inside the nose, mouth and lungs. Every year, genetic mutations in the virus slightly change the chemical flavor of the lollipop, making it more sweet or sour than last season’s — just different enough so the immune system doesn’t recognize it. That’s why most years there’s a new flu shot.
Sometimes, in the gene shuffling with viruses in birds and pigs, the changes are so great that the flavor changes completely. Those are pandemic years, when there is so little residual immunity that a large portion of the global population falls ill from the new virus. The devastating 1918 flu, which killed an estimated 50 million people globally, was caused by such a drastic genetic shift (SN Online: 4/29/14). The most recent pandemic occurred in 2009, with the appearance of the “swine flu,” so named because the virus was first found in pigs. By one analysis, it caused between 148,000 and 249,000 deaths around the world.
Attack the stem
The 2009 disaster helped provide a blueprint for some of the latest experimental vaccines. Researchers noticed that when people with swine flu developed antibodies to the virus, those antibodies did something odd: They favored the hemagglutinin stem — the stick of the lollipop. And, more important, they appeared to react broadly against two kinds of flu virus. Scientists had known that the hemagglutinin stem, or stalk, isn’t as apt to change as the lollipop top, which theoretically makes the stem a good target for a universal vaccine. But in a usual flu season, the human body isn’t inclined to make infection-fighting antibodies against the stem.
“Unfortunately, the immune system preferentially recognizes the head, and we don’t know why it does that,” says Adrian McDermott, an immunologist at NIAID. So after infection, the biggest share of antibodies flocks to the hemagglutinin head. (Neuraminidase, the bigger player in disease after infection, is a target for influenza treatments but not a major focus for vaccine development.)
But in a study reported in the Journal of Experimental Medicine in 2011, a team of scientists from Emory and elsewhere found that antibodies to the so-called swine flu behaved unexpectedly. “If you have a head that the immune system hasn’t seen, you potentially redirect to a stalk response,” McDermott says. “That was an aha! moment.”
Researchers investigated further. For one study in 2012 in Frontiers in Immunology, scientists from Canada injected these stem-recognizing antibodies into mice to see if the mice were shielded from a different strain of flu. Not only were the mice protected from lethal doses of flu virus, but the protection was also in large part due to the absence of familiar antibodies against the head, the researchers found. Without the distraction of a head it recognized, the immune system seemed to rally against the stem.
Then came the what ifs: What if a vaccine produced just antibodies to the stem? Would that be enough protection? For the last few years, McDermott and others have been trying to develop vaccines made of “headless stalks” — just the sticks of the lollipops. With no head in place to hoard the immune response, the vaccine might coax the body to make enough stem-focused antibodies to protect against flu, the researchers hoped, regardless of the seasonal mutations occurring at the top.
Several groups soon found that headless stalks are difficult to make. Without the top to stabilize it, the molecular assembly tended to break apart. Two teams working independently reported in 2015 their success in keeping the stalk in one piece. NIAID scientists and their partners held the stalks together by anchoring them to the protein ferritin, which can assemble itself into nanoparticles. In a study in Nature Medicine, the team reported that vaccinated mice and ferrets appeared to be protected from dying of the H5N1 bird flu after receiving the vaccine, even when they developed symptoms. Unvaccinated mice and ferrets died.
The second team, from the Janssen Center of Excellence for Immunoprophylaxis in Leiden, the Netherlands, and the Scripps Research Institute in La Jolla, Calif., glued the stalk together by creating a series of genetic mutations at its top. In Science, the researchers reported that the vaccine reduced the symptoms of flu in vaccinated monkeys.
“We realized that the stem has much less variability than the head, and then we developed the capability to use it for a possible vaccine,” says Fauci, commenting on both efforts. “These were two important things that came together.”
Despite progress, these stalk-focused vaccines haven’t yet been put to human tests that would show whether they could protect broadly against many mutations of flu circulating annually, which is the ultimate test. And some stalk-directed antibodies might be better than others. In July in Science Immunology, McDermott and colleagues reported that the stalk antibodies against group 2 of the A viruses appear to be more broadly effective than those against group 1 viruses.
Other researchers have stabilized the stalk by attaching a new hemagglutinin head — a lollipop flavor that the human immune system has never tasted. In this case, researchers from the Icahn School of Medicine at Mount Sinai in New York City took tops from two flu strains that circulate only in birds, and connected each one to a human hemagglutinin stalk. This experimental vaccine consists of two doses. The first dose prompts the immune system to make antibodies against the stalk with the first top, and a second dose produces a second round of antibodies against the stalk with the second top. The idea is that the abundance of stem-focused antibodies — amplified from the two shots of vaccine — will come to the rescue during a natural infection from a virus that possesses a third, totally different head.
“The human immune system will try to find something it has seen before,” says Peter Palese, chairman of microbiology at Mount Sinai. In theory, the only antibodies in play will be the ones responding to the parts of the stalk that the immune system recognizes, known as the “conserved domains.”
“The $64,000 question,” according to Palese: “Will the immune response to these conserved domains be enough to elicit a broad immune system reaction?”
In 2016, Palese and colleagues described a test of the vaccine in the Journal of Virology. Six ferrets given the two doses were housed with six ferrets infected with H1N1 flu. Within 10 days, the vaccinated animals had become infected but had no symptoms or signs of being able to easily spread virus to others. A report in June in the same journal described tests of the vaccine in mice against influenza B viruses; the animals were protected from normally lethal doses of flu.
What’s not known is whether the stem-focused antibodies are enough to protect people from all virus variants. The vaccine from the Mount Sinai researchers is entering the first human safety trials with drugmaker GlaxoSmithKline.
Unhide and seek
Another approach incorporates proteins that don’t tend to mutate like the hemagglutinin head but are hidden from the immune system under normal circumstances. When these proteins are made visible to types of white blood cells called T cells, the immune system wakes up. T cells don’t make antibodies, but certain T cells hold on to a memory of foreign molecules seen before. When these pre-programmed T cells recognize an infection, they destroy the invader.
This work began in the 1990s, when researchers at the Weizmann Institute of Science in Rehovot, Israel, set out to find parts of the virus that remain unchanged from year to year. The team identified stable regions in three proteins — hemagglutinin, plus one from the virus membrane and one from the virus core. In 2003, a company called BiondVax Pharmaceuticals formed to develop and test, in humans, an experimental vaccine that takes these proteins and packages them in a way that the immune system can recognize them.
So far, almost 700 volunteers have participated in six small trials, all of which showed signs of a lasting immune response among most volunteers. Writing in February in Vaccine, the researchers reported that the stored serum of elderly volunteers who received the vaccine in 2011 showed an immune response to new strains of flu that were circulating three years later. The company is starting larger trials to see if the vaccine can actually protect people from getting sick.
Out of many, one
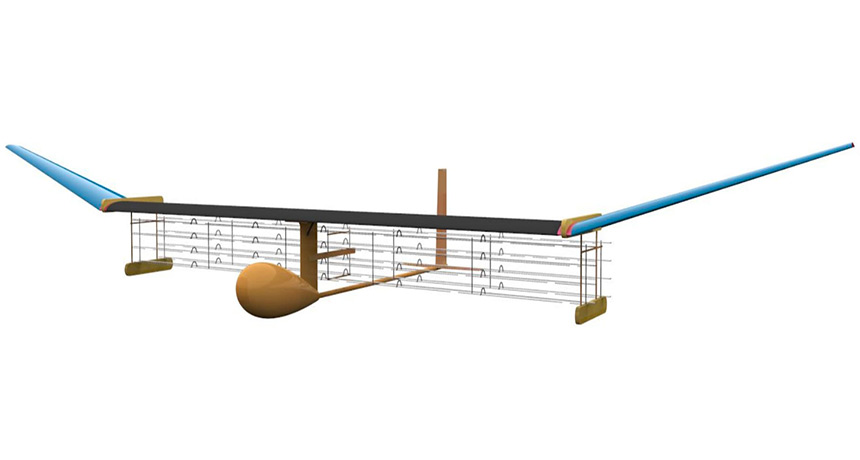
Other experimental vaccines take a different approach. Rather than relying on precision to hit a narrow target, microbiologist Ted Ross and colleagues at the University of Georgia in Athens are attempting to cast a wide net. The researchers are taking hemagglutinin mutations from every flu strain that has ever circulated, dumping them into a kind of scientific blender and attaching them to particles that can form the basis of a vaccine.
“The question we asked is, how can we make a vaccine against a strain we don’t even know exists?” Ross says. The technique he uses is called COBRA for computationally optimized broadly reactive antigen. A computer compiles all seemingly possible genetic iterations of a particular flu type — in this case H1N1 — and then bundles them into one molecule. It’s kind of like taking every novel in your local library and combining them into one giant book.
Last year in the Journal of Virology, Ross and colleagues described a COBRA-derived vaccine that represented almost all forms of H1N1 that have been around for the last 100 years. The vaccine protected mice against infection from strains of H1N1 that the mice had never been exposed to. “We took a bunch of different hemagglutinins and mixed them into one hemagglutinin molecule,” Ross says. “It protected against any strain of H1N1 we could throw at it.”
The study caught the attention of vaccine maker Sanofi Pasteur, which plans to test the vaccine in clinical trials. Ross’ lab is now using the same strategy to develop a vaccine against H3N2 strains, the other dominant kind of flu circulating around the world. Same approach, different library.
Meanwhile, the virus isn’t waiting around. Based on the heavy flu season in the Southern Hemisphere, some experts are predicting this year’s epidemic could be severe. It’s still too early to know whether the current vaccine will provide good protection, but someday, a super shot may remove the guesswork altogether.